What does a statistician know about suicide and suicide prevention?
Said Shahtahmasebi, PhD.
The Good Life Research Centre Trust. Email: radisolevoo@gmail.com
Key words: suicide; suicide prevention; public health; grassroots; depoliticising
Received: 2/2/2018; modified:26/2/2018; accepted: 28/2/2018
[citation: Shahtahmasebi, Said. (2018). What does a statistician know about suicide and suicide prevention? Dynamics of Human Health (DHH), 5(1): http://www.journalofhealth.co.nz/?page_id=1512].
Introduction
Recently, I was made aware of a review of alternative suicide research by a medical modellist. The review lacked academic rigour and was opinionated, and lacked good evidence – so it was not worth reading. However, what caught my attention was the claim made by the reviewer that statisticians and non-psychiatrically trained people are not qualified to engage in suicide research and suicide prevention. It is a claim that is very difficult to take seriously, and is a reflection of the top-down approach to suicide prevention (Shahtahmasebi, 2009). The politicisation of suicide and its prevention and how to depoliticise it is discussed elsewhere (Hjelmeland & Knisek, 2017; Shahtahmasebi, 2013). But, now feels the right time to explore what does anyone know about suicide, and who is qualified to engage in suicide prevention by addressing the following question:
‘What does a statistician know about suicide?’ is the belief of medical modellists who advocate psychiatry and mental illness as the only prevention strategy for suicide.
In this exploratory commentary a distinction is made between those who strongly advocate mental illness as the main cause of suicide and psychiatry in general. For example, a medical modellist asserted the above claim, while a psychiatrist made the following headline: “psychiatrist warns that ‘nothing’ is working in bid to address suicide rates” (Stuff.co.nz, 2017). Clearly, the psychiatrist was referring to the failings of the medical model which has dominated suicide prevention strategy for decades in New Zealand and elsewhere.
Discussion
It may come as a surprise to medical modellists that it was ‘statistics’ (or lack of it) that attracted attention to the flaws in their claims.
Let me describe what a statistician would know about suicide and suicide prevention, and why everyone is qualified to talk about suicide and suicide prevention.
A statistician would know that:
- A good knowledge of statistical concepts and substantive theory are essential to design studies for the collection, analysis and interpretation of suicide data (Shahtahmasebi & Berridge, 2009).
- The suicide case is no longer available to provide information on their process of decision making of choosing death instead of life.
- The public mindset has been shaped by decades of emphasis on mental illness as the reason for suicide (Shahtahmasebi, 2005).
- For example, mental illness is assumed following a suicide incident by association. A good example is of a GP’s comment at a coronial inquest about the suicide of a young high school student who was described as happy, successful both academically and in sport, popular, and had no sign of mental illness:
- “I am desperately sad we had no insight into his mental health problem and so were not able to prevent this tragedy.” (Shahtahmasebi, 2005).
- That is to say, reverse causality is assumed when because the outcome is suicide it is believed that the case must have been mentally ill.
- Therefore, surveys that base the suicide cases’ mental status on families and friends’ post suicide assessment will inevitably inflate the effects of mental illness through measurement error and undue emphasis on the expected outcome (Hjelmeland et al., 2012; Shahtahmasebi, 2005; Shahtahmasebi & Berridge, 2009).
- A major study design flaw is to measure the mental health status of the deceased from a third party(s).
- Worse still, has been the failure to account for such bias in statistical methodologies and interpretation of results leading to spurious results and mis-conclusions (Shahtahmasebi & Berridge, 2009).
- Consequently,
- The claim that 80-90% of suicide cases have a mental illness is an unsubstantiated opinion.
- The claim that suicide is caused by mental illness is tenuous at best.
- Suicide prevention policies based on mental illness as the cause of suicide will not work.
Let’s assume that the selection bias and measurement error and the failure to allow substantive issues do not play a part, and let’s assume further that the medical model is the only way to prevent suicide.
But, after decades of $100s of millions in funding mental health services in order to reduce suicide rates, a statistician knows that:
- If by some miracle there is a link between mental illness and suicide then it will be reflected in the numbers.
- Figure 1 below, shows the long-term trend in suicide rates in New Zealand – it can be seen from this data that there is a bath-tub pattern (a possible long cycle) occurring within which there are a number of smaller cycles.
- Thus suicide rates appear to go down and up independent of any suicide prevention strategy.
- Conflicting trends (see Figure 2, e.g. by age group, gender, and other groups of interest) suggests that there is a lagging effect between groups, e.g. the over 65’s trend is ahead of that of the 45-64’s age groups by an average of three years, and the younger age groups’ suicide trend is almost one cycle ahead so when older people’s suicide rates peaks the younger groups bottoms out.
- If there was a link between mental illness and suicide then a period of sustained ‘suicide prevention’ investment in the mental health services would show a downward trend with some random noise rather than clear cyclic patterns.
- Unashamedly, credit is claimed by the medical modellists when suicide falls compared to previous years, and thus suicide is declared as a complex issue with many social, economic and environmental risk factors when the rate rises!
- In the meantime evidence is piling up that the long-term bath-tub is on its reverse cycle, i.e. if we do not act now we will be faced with a long period of sustained upward suicide rate for years to come.
Figure 1: long-term suicide trends in NZ
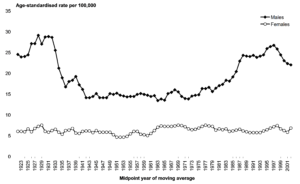
Figure 2: Long-term suicide trends by age group in NZ
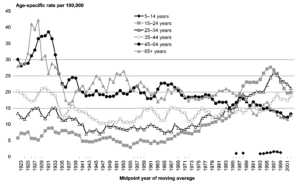
Source: New Zealand Health Information Service
Let’s assume that the data and trends (which are similar for most countries) are nonsense and that the data was not collected properly, then the medical modellists may have a case to claim that mental illness is the only way to prevent suicide.
However, after decades of additional investments in mental health services in order to reduce suicide rates, a statistician knows that:
- Governments around the world including New Zealand invest $100s of millions in mental health services that are tagged for suicide prevention.
- If by a miracle there is a link between mental illness and suicide then we should have had a substantial return on our investments in the number of lives saved and therefore a continuous drop in the suicide rate:
- No such trends can be observed for New Zealand.
- Between 1997-2005 the New Zealand Government’s own reports showed that antidepressant prescriptions had doubled (Ministry of Health, 2007), and then doubled again between 2006-2012 (Antidepressant use in New Zealand doubles, 2012).
- Surely, we should have noticed a drop in suicides by now:
- Unfortunately, during the same period and beyond – suicide rates in New Zealand maintained an overall upward trend!
- [suicide rose to a record high in 2014-15, and again in 2015-16, and again in 2016-17, and the solution each time was investing more millions in mental health (Shahtahmasebi, 2017)].
- [A zero suicide rate was recorded following the earthquakes in Canterbury in 2011with a warning that it would rise again. While medical modellists and policy makers sat on their hands and waited for signs of mental illness to develop – suicide in Canterbury rose and now boasts the highest suicide rate in New Zealand (Shahtahmasebi, 2017)].
- The NZ Suicide prevention strategy has gone unchecked by the taxpayer and is unevaluated by the funders.
Despite having an upward suicide trend that demands ever increasing resources the NZ suicide prevention strategy has been to look for signs of mental illness, depression and make referrals to mental health services.
Basic statistical thinking tells us that after decades of spending millions per year on mental health services to reduce suicide have not led to commensurate reductions in suicide.
A statistician knows that:
- Waiting for symptoms to develop or for the first failed suicide attempt is NOT prevention.
- If signs of mental illness are detected then an event has occurred – so it is time for intervention!
- Mortality data indicates that between one-quarter and one-third of all suicides sought intervention but went on to complete suicide while receiving treatment or soon after discharge from hospital (Hamdi et al., 2008; Ministry of Health, 2016; Shahtahmasebi, 2003).
- This approach ignores the majority of people who don’t exhibit symptoms, or don’t have them, or are good at hiding them
- Between two-thirds and three-quarters of all suicide cases had no contact with medical services – This approach classes this group as mentally ill
- Thus reinforcing the taboo status of both mental illness and suicide.
Let’s assume that a statistician’s knowledge is based on a personal opinion, on that basis the World Health Organisation must be wrong too as in 2014 they described as a myth the claim that all suicide is caused by mental illness (WHO, 2014).
What else do medical modellists claim as to why a statistician is not qualified to comment?
Ah, yes: risk factors of suicide. Medical modellists tell us to look for signs of mental illness including previous suicide attempt(s).
In the context of suicide prevention this is completely wrong. When a suicide attempt is made then the suicide strategy has failed, but alarmingly some people will succeed either at the first attempt or subsequent attempts. This means that previously failed attempts are the outcome of the suicide prevention strategy rather than a suicide risk factor.
It also means that the medical modellists not only failed to prevent suicide but failed multiple times for those cases who made multiple attempts.
Where is the wisdom in waiting for someone to attempt suicide and then use that outcome as a risk factor in order to prevent it?
We do know that medical modellists fail in over two-thirds of suicide cases as they succeed the first time.
Where is the wisdom in persisting on a path that has not produced desirable outcomes (Hjelmeland & Knisek, 2017).
Conclusion
What else would a statistician know about suicide prevention? Ah yes, in any other setting, be it private or public, the inability to produce desired results, given the massive year upon year investment, would have led to heads being rolled, a re-evaluation and change in staff, and a redirection. In any other setting the taxpayer would have demanded to know what has happened to the millions given to mental health services for suicide research and suicide prevention. Why have suicide rates not fallen?
It appears that politics and vested interests could explain, at least in part, the reasoning and logic behind our love affair with the medical model which does not prevent suicide (Hjelmeland & Knisek, 2017; Shahtahmasebi, 2013).
However, one thing that medical modellists including the government would not know is that how effective, inexpensive and sustainable grassroots suicide prevention, developed by a statistician, can be (Shahtahmasebi, 2013).
My message to the medical modellists is this: 2015 and 2016 and 2017, and if their memory stretches further than a year ago the ‘Canterbury earthquake experience’. If these do not make sense to medical modellists then they should either study statistics, or brush up on their psychiatric knowledge and substantive theory, or all of the above (Shahtahmasebi & Berridge, 2009). In other words, they should not be in the ‘business’ of suicide prevention.
I guess the table has turned and the question on the grassroots’ lips is can medical modellists tell us anything new about suicide and suicide prevention?
At the end of the day, it doesn’t matter how right or wrong a policy is it won’t work if it doesn’t have the backing of the people at grassroots; medical model does not.
References
Antidepressant use in New Zealand doubles. (2012). The government’s drug-buying agency, pharmac, says it is monitoring the growing use of anti-depressants in new zealand. http://www.radionz.co.nz/news/national/117826/pharmac-monitoring-use-of-anti-depressants.
Hamdi, E., Price, S., Qassem, T., Amin, Y., & Jones, D. (2008). Suicides not in contact with mental health services: Risk indicators and determinants of referral. J Ment Health, 17(4), 398-409.
Hjelmeland, H., Dieserud, G., Dyregrov, K., Knizek, B. L., & Leenaars, A. A. (2012). Psychological autopsy studies as diagnostic tools: Are they methodologically flawed? Death Studies, 36(7), 605-626.
Hjelmeland, H., & Knisek, B. L. (2017). Suicide and mental disorders: A discourse of politics, power, and vested interests. Death Studies, 41, DOI: 10.1080/07481187.07482017.01332905.
Ministry of Health. (2007). Patterns of antidepressant drug prescribing and intentional self-harm outcomes in new zealand: An ecological study. Wellington: Ministry of Health.
Ministry of Health. (2016). Office of the director of mental health annual report 2015. Wellington: Ministry of Health.
Shahtahmasebi, S. (2003). Suicides by mentally ill people. ScientificWorldJournal, 3, 684-693.
Shahtahmasebi, S. (2005). Suicides in new zealand. ScientificWorldJournal, 5, 527-534.
Shahtahmasebi, S. (2009). Suicide prevention in a top-down society. In L. Sher & A. Vilens (Eds.), Suicide in the military (pp. 121-136). New York: Nova Sci.
Shahtahmasebi, S. (2013). De-politicizing youth suicide prevention. Front. Pediatr, 1(8), http://journal.frontiersin.org/article/10.3389/fped.2013.00008/abstract.
Shahtahmasebi, S. (2017). Editorial: Suicide numbers a record high for the third year running. Dynamics of human health (DHH), 4(3), http://www.journalofhealth.co.nz/?page_id=1160.
Shahtahmasebi, S., & Berridge, D. (2009). Conceptualising behaviour in health and social research: A practical guide to data analysis. New York: Nova Sci.
Stuff.co.nz. (2017). Psychiatrists warn that ‘nothing’ is working in bid to address suicide rates. http://www.Stuff.co.nz/national/health/96946527/canterbury-suicide-rate-worrying-psychiatrist-warns-nothing-is-working?cid=facebook.post.96946527.
WHO. (2014). Preventing suicide: A global imperative. http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/.