Modelling nutritional intervention with application to suicide prevention
Said Shahtahmasebi, PhD
The Good Life Research Centre Trust, Christchurch, New Zealand.
Correspondance: radisolevoo@gmail.com
Key words: holistic modelling, nutrition, suicide, prevention
Received: 15/7/2019; revised 2/9/2019; Accepted: 15/9/2019
[citation: Shahtahmasebi, S. (2019). Modelling nutritional intervention with application to suicide prevention. DHH; 6(3):http://www.journalofhealth.co.nz/?page_id=1881].
A holistic view of human life to address individuals’ and social problems is not a recent phenomenon. It dates back to the time of ancient philosophers and prophets. For example the Persian philosopher/prophet Zoroast’s ideology and training was based on an holistic view of both the physical and mental status; being good must come from thinking good and doing good deeds. Clearly, these instructions are inter-linked through “feed-back” links. Similarly, variations of the Ten Commandments, common in most religions instruct deeds that lead to goodness. These are not merely instructions but a holistic approach to culture and social harmony. Although, they guide individuals to be good and to do good deeds, the overall feedback effect is intended to benefit society and communities when all the individuals follow the same philosophy in achieving a spiritually, mentally and physically healthy society.
It is these ideologies that influenced many subsequent philosophers and practitioners who adopted the approach of considering the whole ‘person’ when treating an illness. The argument behind such an approach has been that physical symptoms could often be the manifestation of underlying (unobserved) mental (and spiritual) problems and vice versa. Therefore, the interaction between physical, mental and spiritual elements must be present in the treatment of an illness.
The practice of treating the whole body can only be holistic if all the feedback links are operational. For example, it wold hardly be holistic to attend to body and mind while the social, economic, family environment, and other processes are left unattended, ignored or unchanged.
However, there have been many cases which have utilised such a relationship with a positive outcome. The following case history would perhaps demonstrate the application of the concept of treating the “whole” person more explicitly.
In a case (M. Shahtahmasebi, 1985) the patient had exhibited psychological symptoms: mainly believing that he possessed mythical and supernatural powers:-
He insisted on shifting the rocky mountains on the outskirts of the city with his bare hands. His family had consulted well-known consultants and specialists and all manner of tests had been conducted and treatments had been prescribed. By the time the last resort was called upon the patient was in a bad shape; he was emaciated and skeletal, was tied down to the bed for his own safety. The family explained that they had tried everything and that they had heard about the doctor’s healing powers – and they were hoping for a miracle. After checking the patient’s and his family’s history, the doctor asked for the patient to be untied. He told the patient that he had come for his help to shift the rocky mountains and had heard that he (the patient) is the only one that could help. To the horror of the family he helped the patient to get organised and they walk towards the front door. The doctor reached for the door handle but before turning it open he turned to the patient and said “let’s shake on our new partnership!” The doctor squeezed the patient’s hand so that the patient complained of pain. The doctor persuaded the patient since his hands are important for this mission they both should have something to eat and then try again the next day. The patient voluntarily goes back to his room and waits to be fed. In the meantime the doctor makes up a comprehensive prescription mainly dietary. The same pattern of events followed the next day and the next and the next and so on. On what became the final visit, the doctor turned up at the house and examined the patient and said that he was now strong enough to go ahead and help shift the mountains, to which the patient responded “why?, are you crazy doctor!”
In the final analysis the holistic treatment realigned the patient’s feedback links to himself and his family and community which had led to disruption in his dietary pattern and subsequent psychological symptoms.
With population growth and environmental and evolutionary changes, health care systems have become more and more complex in order to respond to ill-health needs of the population. This interventional approach has led to a perpetual conveyor belt system where patients enter the health care system, their apparent symptoms are addressed and subsequently leave, and then re-enter some time later. The fable of the physician on the river bank may describe the problem more clearly, retold by McKinlay (McKinlay, 1975), though attributed by him to Irving Zola:
“you know”, he said, “sometimes it feels like this. There I am standing by the shore of a swiftly flowing river and I hear the cry of a drowning man. So I jump into the river, put my arms around him, pull him to the shore and apply artificial respiration. Just when he begins to breathe, there is another cry for help. So I jump into the river, reach him, pull him to shore, apply artificial respiration, and then just as he begins to breathe, another cry for help. So back in the river again, reaching, pulling, applying, breathing and then another yell. Again and again, without end, goes the sequence. You know, I am so busy jumping in, pulling them to shore, applying artificial respiration, that I have no time to see who the hell is upstream pushing them all in.”
Thunhirst (Thunhirst, 1982) argued that we have spent too long measuring the flow of the river, the size of the fishing nets and the rate at which people are brought to shore. Health statisticians and health professionals need to refocus, Thunhirst argues, to investigate the largely unmapped terrain upstream – particularly in solving the problem of differential class experiences of health.
In essence, even with a fundamental shift in our approach to understand and resolve a problem we are still parameterising the problem not in an abstract mathematical fashion but rather more qualitatively, without attempting to explore the reasons why the problems exist in the first place. Without a good insight into the problem (e.g. disease) the development of possible solutions may become part of the problem in a short period of time.
It is all very well to conceptualise and map out a particular issue such as human health, but without insight into the dynamics of human health it is almost impossible to translate it into a sustainable action plan. Health outcomes are closely related to nutrition and diet which have evolved, amongst other processes, through environmental processes, agriculture, individual’s choice and palate, income, culture, transport and access, nutritional knowledge and information. For example, Wilkinson (Wilkinson, 1976), after a two stage data dredging, concluded that dietary factors were closely related to mortality rates, and that differentials in mortality due to class may well be determined by differences in diets which are the most important socio-economic factors. The link between nutrition/diet and health is well documented (Townsend & Davidson, 1982).
Population health is, therefore, a function of governments’ health, social, economic, agriculture, and environmental policies, which are often about allocating and distributing resources within an interventional health care system. Thus, one of the persevering issues, inevitably, has been optimisation, e.g. maximising services and/or service delivery given available funds. In the past, attempts have been made to formulate nutrition, in particular with reference to the low income groups and third world countries by optimising costs. Because, optimisation seeks to maximise quantities of ingredients for the available funds, it leads to a single point solution which gives maximum quantity for minimum costs. Such a solution results in food items that consist of much higher quantities of cheaper ingredients which are of low nutritional value than ingredients with high nutritional value in order to meet costs. Thus, optimisation is not suitable for modelling the nutritional needs of human beings.
Policy implications
Conceptualising the optimisation of nutritional values of food rather than costs is more relevant to human health. However, such modelling poses several problems, for example, firstly, the outcome may lead to solutions that are financially prohibitive. Secondly, it may, lead to solutions that lead to over feeding which could be harmful to human health.
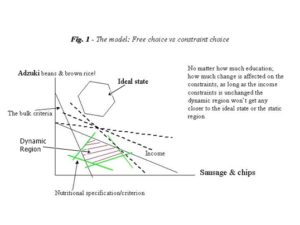
We all require nutritional elements in order to survive and function. However, the quantity required may vary from individual to individual; but generally, the consumption of most of the nutritional elements may be bounded by an upper and/or lower constraints, such as the minimum and maximum daily recommended allowance for fat, sugar, calcium, minerals, vitamins and so on. These upper and lower bounds will form a region that could be assumed to be the ideal state (see Fig. 1). In other words, the interest is no longer in finding a single point that minimises costs; any point in the ideal region can be assumed a valid solution, e.g. food items or dietary patterns that meet the nutritional requirements of individuals. However, the actual nutritional intake is bounded by individuals’ characteristics, income, dietary patterns, access, transport, choice of food, quantity, nutritional values, and so on, which form a different region. This new region can be assumed dynamic because the bounds are under the control of individuals thus they vary between and within individuals (see Fig. 1). In practice, it may be the case that the actual nutritional intake of some individuals will overlap with the ideal state or no overlap at all.
Policy analysis
Such a conceptualisation will have implications for policy formation and evaluation. For instance, we could consider developing policies that influence the movement of the dynamic region towards the ideal region to achieve at least a partial overlap.
In order to affect public health positively, we can influence these social and environmental bounds to achieve an overlap, i.e. where the actual nutritional intake of the public will meet, at least in part, the recommended intake. The questions are what actions can influence a shift in the dynamic region towards the ideal state, and by how much? On the other hand, how can we be sure that changes in boundaries, e.g. income, education, and access will directly lead to a shift in the dynamic region towards the ideal state?
Discussion
We know that low income households and people with financial difficulties they always cut back on food (Lang, Andrews, Bedale, & Hannon, 1984). The case of the single mother on a low income comes to mind. For those on low incomes it is not unusual to cut back on food on a regular basis or go without food at least once a week (e.g. see (Lang et al., 1984)). The single mother in question was a typical case. When she spent the additional money she earned from taking part in an interview on a hair-do there was an outcry from the researchers! The expectation was that the respondent would spend the money on food for her children. This example highlights: firstly, the differentials in perceptions and expectations between the subjects and the researchers (as utilised by (Ackoff, 1970)). Secondly, that we tend to overlook social, mental and spiritual wellbeing which define overall health in favour of physical health when considering the health of the public.
Implications
A dynamic approach to map out the problem being modelled as that of individuals in contrast with established ideals will assist in conceptualising strategies that could lead to beneficial action plans.
For example, the above model can be used to conceptualise suicide prevention which has persistently outsmarted governments, and develop strategies that will have an effect on annual suicide rates (S. Shahtahmasebi, 2013).
To conceptualised a suicide prevention strategy we need to gain insight into suicide. The suicide literature that has been used to inform suicide prevention policies have mainly been based on the idea that mental illness is the cause of suicide. However, there is a growing body of evidence to dismiss the medical explanation of suicide (Hjelmeland, Jaworski, Knizek, & Marsh, 2018; Hjelmeland & Knizek, 2017; Pridmore, 2011, 2014; Pridmore & Walter, 2013; S. Shahtahmasebi, 2003, 2005, 2013) but most damning has been the annual suicide rates (e.g. see (Pridmore & Shahtahmasebi, 2018)); not only trending upward despite governments’ suicide intervention strategies, but also for suicide rates following a cyclic pattern.
The first problem is that a period of falling suicide rates leads to complacency setting in, but when the rates rise it is often considered a blip in the time series. So, instead of redressing their approach to suicide prevention governments persevere with the same failed policies until the next period where rates fall. This strategy has led to “more of the same” mental illness intervention policies, thus exacerbating the problem of suicide prevention.
The second problem is the literature has not explicitly proven cause and effect, e.g. mental illness causes suicide. Instead, the literature subdivides the public into many groups with adverse life experiences, including various mental illness categories, those with failed relationship or break ups, bereaved, unemployed, with financial hardship, and so on, as being at suicide risk. The problem is that people without a mental illness, the employed, the well off, and so on, also suicide. Suicide prevention is discussed in detail elsewhere (S. Shahtahmasebi, 2013).
Despite decades of failing to reverse the rising suicide trends, very little research has been conducted to understand suicide as a human behaviour outcome.
Using such a conceptual model will guide the direction of research. For example, whether it is modelling nutrition, suicide, or another issue, a good understanding of human behaviour is absolutely essential (S. Shahtahmasebi, 2006, 2013).
References
Ackoff, R. (1970). A black ghetto’s research on a university. Operations Research, 18, 761-771.
Hjelmeland, H., Jaworski, K., Knizek, B. L., & Marsh, I. (2018). Problematic Advice From Suicide Prevention Experts. Ethical Human Psychology and Psychiatry, 20(2), 79-85.
Hjelmeland, H., & Knizek, B. L. (2017). Suicide and Mental Disorders: A Discourse of Politics, Power, and Vested Interests. Death Studies, 41, DOI: 10.1080/07481187.07482017.01332905. doi: DOI: 10.1080/07481187.2017.1332905
Lang, T., Andrews, H., Bedale, C., & Hannon, E. (1984). Jam Tomorrow? A report of the first findings of a pilot study of the food circumstances, attitudes and consumption of a 1000 people on low income in the north of England: Dept. of Hotel & Catering, Manchester Polytechnic.
McKinlay, J. (1975). A case for refocussing upstream: the political economy of sickness. In A. Enelow (Ed.), Applying behavioural science to cardiovascular risk. New York: American Heart Association.
Pridmore, S. (2011). Medicalisation of Suicide. Malaysian J Med Sci., 18(4), 77-82.
Pridmore, S. (2014). Why suicide eradication is hardly possible. Dynamics of Human Health (DHH), 1(4), http://www.journalofhealth.co.nz/wp-content/uploads/2014/2012/DHH_Saxby_Eradicating-suicide.pdf.