“Trans” means across and “cranial” refers to the cranium or the bone box (skull) which keeps our brain safe. TMS enables the brain to be stimulated (and thereby treated) by gentle surges of electrical energy…
Transcranial Magnetic Stimulation (TMS): Information for those considering treatment.
Saxby Pridmore 1, Marzena Rybak 2, Yvonne Turnier-Shea 2, Karen Byrne 2, Tae Dillon 2, Ahmed Naguy 3
1 Discipline of Psychiatry, University of Tasmania, Tasmania, Australia; 2 TMS Hobart, Bellerive, Tasmania, Australia; 3 Kuwait Centre for Mental Health, Shuwaikh, State of Kuwait.
Correspondance: Prof S Pridmore, email: s.pridmore@utas.edu.au
Received: 31/05/2024; Revised: 14/06/2024; Accepted: 18/06/2024
Key words: Major depressive disorder; Depression rating scales; quantifying mood experience.
[citation: Pridmore, Saxby; Shahtahmasebi, Said; Turnier-Shea, Yvonne; Rybak, Marzan; Naguy, Ahmed (2024). Transcranial Magnetic Stimulation (TMS): Information for those considering treatment. Dynamics of Human Health (DHH), 11(1):https://journalofhealth.co.nz/?page_id=3091].
Introduction
Transcranial Magnetic Stimulation (TMS) has been studied and used in the treatment of major depressive disorder (MDD) for three decades [1].
“Trans” means across and “cranial” refers to the cranium or the bone box (skull) which keeps our brain safe. TMS enables the brain to be stimulated (and thereby treated) by gentle surges of electrical energy. This electrical activity is placed where it is needed using magnetism. If you put a paperclip on a table and a magnet underneath, you can move the paperclip by moving the magnet. In the same way, magnetic forces can pass across the skull and place electrical stimulation in precise sites. We will return to the nature and effects of TMS shortly.
Some brain structures
The brain is an amazingly complex structure. It contains different types of cells – but we will only discuss one – the most common type – the neuron. Amazingly, we each have about 100 billion neurons in our brains.
The neuron has three main parts (Fig 1). First, the cell body, which contains the nucleus, which houses DNA and directs the daily activities of the cell. Additionally, the cell body supports fine projections (dendrites) which receives information from connected neurons. Second, the axon – a long, thin component (like telephone wires) which carries impulses (messages) from the cell body to the third part of the cell – the axon terminals. Axon terminals contact distant neurons and pass the impulses on.
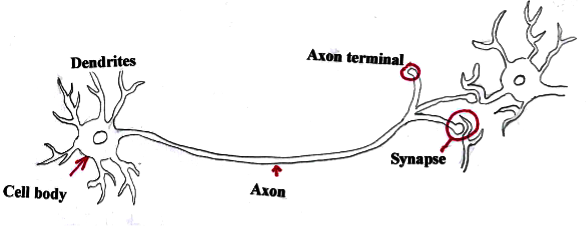
Fig 1. The neuron. Three parts: cell body, axon and axon terminals.
When cell bodies are close, axons may only be millimetres long. In other brain regions they may be centimetres long. [In another part of the body – an axon passing from the spinal cord to the foot, in a tall person, may be one meter long.]
The only other structure we need to consider is the synapse – the connection between two neurons (Fig 2). The axon terminals of a first neuron contact the dendrites of another neuron (occasionally they make direct contact with the cell body). Synapses are highly complex structures and have different forms – depending on the function of the neurons (excitatory, inhibitory, associated with movement, mood, cognition, etc.).
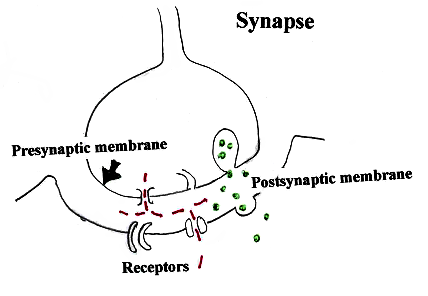
Fig 2. A synapse. Neurotransmitters and ions are released from the presynaptic membrane, pass across the synaptic cleft, are taken up by receptors in the postsynaptic membrane and influence the working of the next neuron.
Buds on the axon terminals have a specialized surface known as the “presynaptic membrane” – the matching area on the dendrite or the cell body is known as the “postsynaptic membrane”. These membranes are not in contact, but separated by a tiny gap called the synaptic cleft. When an impulse/message arrives at the presynaptic membrane, various substances (depending on the nature/function of the neuron) are released into the cleft and are then taken up by specialized/appropriate receptors on the postsynaptic membrane.
These substances include 1) neurotransmitters, and 2) ions (eclectically charged molecules and atoms (such as Ca2+, K2+and Na2+). The neurotransmitters are chemicals such as Glutamate which excites, and Gamma-Aminobutyric Acid which suppresses activity in the next neuron. The ions alter local electrical charges, and thereby modify the activities in various structures – such as increasing the responsiveness of receptors and opening various physiological channels.
Organic basis of MDD
The organic bases of many psychiatric disorders remain unclear. MDD is believed to be (at least in part) due to abnormalities of the synapses (but this is certainly not the complete story). For many years a prominent theory of MDD pathology has been the “monoamine hypothesis” – which states MDD is due to problems (depletions) in levels of the synaptic neurotransmitters serotonin, norepinephrine and possibly dopamine. This has been the basis for most drug treatments of depression.
Reductions in the volume of white and grey matter brain structures have been observed in MDD – it is unclear whether this is a cause or a result of MDD. Also, a disorder of the stress response has been reported in MDD.
Abnormal ‘functional connectivity’ has been observed in MDD – again, whether this is a primary or secondary effect is unclear. Functional connectivity is a relatively new concept/discovery and deserves a little explanation.
Brain regions spontaneously send impulses to each other, via axons. ‘Connectivity’ is the term used to describe the frequency and speed with which these impulses are transmitted. Obviously when there has been brain damage (and axons have been distorted or destroyed) the connectivity of those regions will be impaired.
Functional connectivity is the term applied when connectivity is abnormal, but there is no clear anatomical/physical explanation. In psychiatric disorders there is no clear evidence of axonal damage, but the functional connectivity is frequently abnormal. Specifically, in MDD there is a generalized reduction in connectivity, but with increased connectivity in particular tracts.
TMS basics
When an electric current travels along a wire, a magnetic field extends out at right angles to that current. [Physicists tell us we should not see electric and magnetic phenomena as separate – they are complimentary components of the phenomenon of electromagnetic force.]
When a coil is held on the head and an electric current is applied, a magnetic field extends through the skull into the outer part of the brain directly beneath. When the electric current in the coil is turned on and off, the magnetic field fluctuates in strength – this leads to a fluctuating electric field which stimulates that part of the brain.
If we exercise our arm muscles they change – they become stronger and develop more stamina. Similarly, electrical stimulation of the nervous system can trigger change in structure, connections and responses (this is termed neuroplasticity). TMS can induce extensive neuroplasticity.
Effects of TMS in MDD
Recent advances [2] indicate TMS produces important changes at receptors (synaptic plasticity). It produces changes in the concentration of neurotransmitters and increases and decreases the excitability (tendency to respond) of receptors. TMS also increases to number/availability of receptors.
TMS also modifies connectivity – applied in MDD it simultaneously increases the connectivity of underactive regions and decreases the connectivity of overactive regions [3].
During the TMS treatment of MDD a number of other organic brain changes have been described – but is not clear whether or not these contribute to the clinical response [4].
Treatment setting
A TMS treatment session, using the traditional technique, takes about half an hour. (Some newer stimulation methods may take less than 5 minutes.) The traditional system is one daily treatment (excluding weekends) with a minimum total of 20 treatments – often a course may extend to 35 treatments. In specialized centres, more than one treatment may be provided in one day.
The patient sits or is semi-reclined in a comfortable chair, with a figure-of-eight shaped coil touching the head (Fig 3). The positioning of the coil (left or right of the front of the head) and the number of stimuli delivered per second (“the frequency”) depends on clinical factors. Treatment feels like a tapping on the head. Occasionally a patient may find this experience uncomfortable.

Fig 3. The treatment setting. The patient, the device and the treatment coil.
Side-effects: there is very, very small risk of a seizure. Although seizure is exceedingly rare – people with epilepsy or a strong family history of epilepsy are not treated. The most common side-effect is a mild headache – which (if treatment is necessary) responds to simple pain relief.
Effectiveness
TMS is indicated when medication has not been sufficiently helpful. Some authorities claim TMS is as effective in the treatment of MDD as ECT [5] – this is probably an overstatement, but most certainly, TMS has far less side-effects. One group of experts [6] state routine TMS produces a response (reduction in symptom severity by 50%) in 58-83% of cases, and remission (removal of all symptoms) in 28-62% of cases. A more recent study [7] reports a response rate of 31% and a remission rate of 22.8%. While this is a much less optimistic claim, this report nevertheless indicates that at least half of those who receive TMS for MDD will be relieved of at least half their symptoms.
Approval and reimbursement
TMS has been approved in most countries of the world as safe and effective in the treatment of MDD which has not responded to medication – it is widely available in USA, Canada, UK, France, Portugal, Germany, Finland, Israel, Brazil, New Zealand and Australia.
In Australia TMS receives Medicare Benefits Schedule (MBS) Item Number rebates – that is, TMS treatments have been sanctioned and health care providers can receive government based financial payments for providing this clinical service. To this point there are some rules which are unwelcome by clinicians and patients, such as limitations on the number of treatments which can be rebated – but hopefully these will be resolved in the future. Some private health insurers cover TMS costs, but not all – workers compensation insurers generally cover TMS. To this point, in Australia, some patients are self-funding their treatment.
In short
TMS has been used in the treatment of MDD for three decades. It is suggested as a treatment when medication has failed to relieve symptoms. (In the future it will possibly become a first line treatment.) It facilitates the function of synapses (and various other brain structures) and corrects the connectivity abnormalities of MDD. It has few troublesome side effects and while it does not cure every case, it cures and helps many others.
References
[1] George M, Wasserman E, Williams W, et al. (1995) Daily repetitive transcranial magnetic stimulation improves mood in depression. Neuroreport 6(14): 1853-1856. doi: 10.1097/00001756-199510020-00008.
[2] Fitzsimmons S, Oostra E, Postma T, et al. [2023] Repetitive transcranial magnetic stimulation induced neuroplasticity and the treatment of psychiatric disorders: State of the evidence and future opportunities. Biol Psychiatry 95(6):592-600. doi: 10.1016/j.biopsych.2023.11.016.
[3] Pridmore S, Turnier-Shea Y, Rybak M, et al. (2023). Transcranial Magnetic stimulation for major depressive disorder – Modus operandi. Psychopharmacology Psychopharmacol Bull 53(3): 55-60.
[4] Boylu M, Turan S, Guler E, et al. (2024) Changes in neuroactive steroids, neurotrophins and immunological biomarkers after monotherapy 8-week rTMS treatment and their relationship with neurocognitive functions in depression. Eur Arch Psychiatry Clin Neurosci 274(4):849-865. doi: 10.1007/s00406-023-01704-9.
[5] Ontario Health (Quality). (2021) Repetitive Transcranial Magnetic Stimulation for people with treatment-resistant depression: A Health Technology Assessment. Ont Health Technol Assess Ser 21(4):1-232. eCollection 2021.
[6] Sackeim H, Aaronson S, Carpenter L, et al. (2020) Clinical outcomes in a large registry of patients with major depressive disorder treated with Transcranial Magnetic Stimulation. J Affect Disord 277: 65-74. doi: 10.1016/j.jad.2020.08.005.
[7] Bouaziz N, Laidi C, Bulteau S, et al. (2023) Real world transcranial magnetic stimulation for major depression: A multisite, naturalistic, retrospective study. J Affect Disord 326: 26-35. doi: 10.1016/j.jad.2023.01.070